KIR genotype
& HLA testing
KIR molecules, HLA ligands and infertility
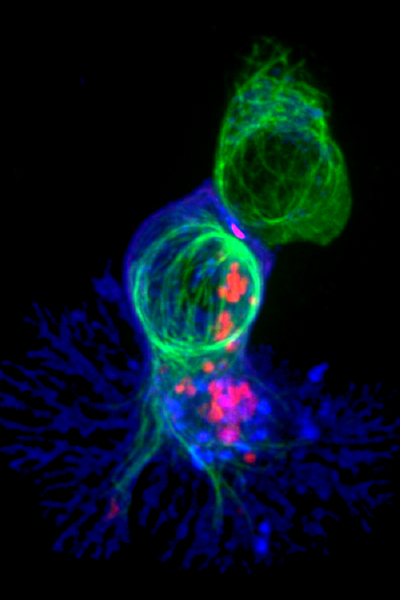
KIR molecules are proteins found on natural killer cells that interact with HLA molecules on the surface of cells to help the immune system identify and respond to different types of cells, ensuring the body's health and safety.
KIR stands for Killer-cell Immunoglobulin-like Receptor. KIR molecules are proteins found on the surface of certain immune cells called natural killer cells (NK) cells. These molecules help the immune system identify and respond to different types of cells in the body.
KIR molecules have a specific job: they recognize and interact with other molecules called HLA (Human Leukocyte Antigen) molecules. HLA molecules act as name tags on the surface of our body’s cells. They help the immune system distinguish between our own cells and cells that may be foreign or harmful, such as viruses or cancer cells.
When KIR molecules on natural killer cells encounter HLA molecules on the surface of cells, they form a connection or interaction. This interaction helps the natural killer cells determine whether the cells they encounter are healthy and belong to our own body or if they are potentially dangerous or infected.
For example, if a cell in our body is infected with a virus and its HLA molecules display certain changes, the KIR molecules on natural killer cells can recognize those changes. This recognition signals the natural killer cells to take action and destroy the infected cell to protect the body from further harm.
KIR genotype and infertility
The KIR genotype has been studied in relation to infertility, particularly in the context of reproductive disorders such as recurrent miscarriage and implantation failure in assisted reproductive technologies (ART).
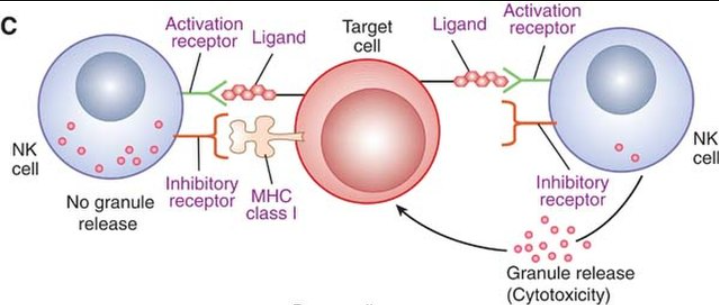
KIRs are found on natural killer (NK) cells and some subsets of T cells. They play a crucial role in regulating immune responses, particularly in recognizing and interacting with human leukocyte antigen (HLA) molecules on target cells.
HLAs are groups of proteins present on the surface of our cells. They bind specifically with the KIR molecules found on NK cells. The interaction between KIRs and HLA molecules influences the function and activity of NK cells. There are different types of KIR molecules and HLA ligands which all have varying affinities for each other. When an HLA ligand binds to its corresponding KIR receptor, it can either activate or inhibit the NK cell.
Types of KIR molecules
There are two main groups of KIR receptors based on their structure and function.
Inhibitory KIRs: These receptors transmit inhibitory signals to the natural killer (NK) cell when they bind to their specific HLA ligands. They help in distinguishing healthy cells from infected or abnormal cells.
Activating KIRs: These receptors transmit activating signals to the NK cell upon binding to their ligands. They play a role in recognizing stressed, infected, or cancerous cells. This binding triggers an activation signal in the NK cell, leading to the destruction of the targeted cell.
The balance between activating and inhibitory signals from KIR receptors and HLA ligands is crucial for maintaining proper immune responses. Alterations in HLA ligand expression or KIR receptor function can impact the recognition and elimination of target cells, potentially affecting our body’s immune surveillance.
KIRs and infertility
Several studies have suggested that specific combinations of KIR genes and their corresponding HLA ligands may be associated with reproductive disorders and infertility. The presence or absence of certain KIR genes and their HLA ligands may affect the maternal-fetal immune interaction during pregnancy, potentially leading to implantation failure or recurrent miscarriage.
One of the well-studied KIR genes in relation to infertility is KIR2DL2/2DL3, which recognizes HLA-C group 1 ligands. Some studies have reported an association between the presence of KIR2DL2/2DL3 and their HLA-C group 1 ligands with an increased risk of recurrent miscarriage.
On the other hand, the presence of KIR2DL1, which recognizes HLA-C group 2 ligands, has been suggested to have a protective effect against miscarriage.

HLA molecules and infertility
HLA has been studied in relation to reproductive disorders, particularly in the areas of implantation failure and recurrent miscarriage.
HLA compatibility – Some recent studies suggest that, just as HLA matching is crucial in organ transplantation to minimize the risk of rejection, similarly, HLA compatibility between partners could potentially influence fertility outcomes, including the success of in vitro fertilization (IVF) and the occurrence of recurrent miscarriages. Research is continuing in this area to determine how significant a factor HLA matching is to fertility outcomes.
HLA-G expression – Furthermore, one specific HLA molecule, the HLA-G molecule, has been found to have immunomodulatory properties. It is primarily expressed in the placenta during pregnancy and is involved in maternal-fetal immune tolerance. It is thought to play a role in successful implantation and pregnancy maintenance. Recent studies have examined the association between various forms of HLA-G molecules and fertility outcomes, with some suggesting a potential link between some HLA-G variants and reproductive success. However, more research is necessary to confirm these findings and fully understand the implications.
HLA and autoimmune disorders – Also, it is worth mentioning here that, certain autoimmune disorders, such as systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS), are known to affect fertility. These conditions are characterised by the presence of autoantibodies that can target HLA molecules and interfere with normal immune responses, potentially leading to reproductive complications

our story Signs of an abnormal immune system
Abnormal immunological reactions during pregnancy can lead to a variety of complications that may affect both the mother and the developing fetus.
Such immune reactions may not always cause symptoms that are noticeable to the mother. In other cases, an immune reaction can lead to symptoms including Recurrent miscarriage, Abnormal vaginal bleeding, Abnormal placenta development, Preterm labor, Intrauterine growth restriction and others.
HLA testing and treatments for infertility
While HLA testing is not commonly performed as a standard diagnostic tool for infertility, it may be considered in specific cases where there is a suspected immune-related cause or a history of recurrent pregnancy loss.
HLA ((Human Leukocyte Antigen)) testing, specifically HLA matching between partners, can provide valuable information in cases of infertility, particularly in the context of reproductive medicine techniques such as in vitro fertilization (IVF) and intrauterine insemination (IUI). It is a specialised area of reproductive immunology and research is continuing.
Recent studies indicate that HLA testing may be helpful in several areas of infertility investigation, particularly in the assessing of:
Immunological compatibility: HLA molecules play a critical role in the immune system and can influence the success of pregnancies. In some cases, a woman’s immune system may recognize her partner’s sperm or embryos as foreign due to differences in HLA profiles. This can trigger an immune response that may lead to implantation failure or miscarriage. By assessing the HLA compatibility between partners, it can help to identify potential immunological barriers and plan appropriate treatments to mitigate immune-related infertility issues.
Natural killer (NK) cell activity: NK cells are immune cells that play a role in the implantation process by regulating the formation of blood vessels in the uterine lining. Imbalances in NK cell activity, particularly overactivity, have been associated with recurrent pregnancy loss and infertility. HLA compatibility between partners can affect NK cell function. HLA testing can help identify any HLA mismatches that may contribute to altered NK cell activity, and this can be used to develop personalised treatment approaches such as immune-modulating therapies, to optimise the chances of successful pregnancy.
Preimplantation genetic testing: Preimplantation genetic testing (PGT) is a technique used during IVF to screen embryos for genetic abnormalities before implantation. In some cases, HLA testing can be performed alongside PGT to identify embryos that are not only genetically healthy but also HLA-compatible with a sibling or a parent requiring hematopoietic stem cell transplantation (HSCT).
HLA Testing
HLA Typing
HLA typing involves analyzing the genetic makeup of HLA molecules, particularly HLA class I and II genes. This testing can be done for both partners to assess the compatibility of their HLA alleles. HLA compatibility or incompatibility between partners has been investigated as a potential factor in recurrent miscarriages.
HLA Antibody Testing
HLA antibody testing involves assessing the presence of antibodies against HLA molecules. This testing is primarily used to evaluate the potential impact of immune responses against HLA molecules on pregnancy outcomes. The presence of certain HLA antibodies, especially anti-HLA class I antibodies, has been associated with an increased risk of recurrent miscarriages. Testing for HLA antibodies may involve techniques such as solid-phase assays or flow cytometry-based methods.

Treatment Options
In cases where immune-related factors, including HLA-related factors, are suspected to contribute to recurrent miscarriages, immunomodulatory therapies may be considered. These therapies aim to modulate the immune response to improve pregnancy outcomes. Treatments can include the use of medications such as corticosteroids, intravenous immunoglobulin (IVIg), or other immunosuppressive agents.
The management of recurrent miscarriages may involve other approaches depending on the underlying causes identified through comprehensive evaluation. These can include addressing hormonal imbalances, surgical interventions for anatomical issues, genetic counseling and testing for chromosomal abnormalities, or treatments targeting specific reproductive disorders or infections.
HLA-DQ alpha compatibility and infertility
Some studies have suggested a potential link between HLA-DQ alpha compatibility and infertility. Specialised diagnostic testing for DQa (HLA-DQ alpha) can be done as part of a fertility investigation if indicated.
DQa (HLA-DQ alpha) testing involves analyzing the genetic variants or alleles of the HLA-DQ alpha gene. This type of testing is typically performed in the context of organ transplantation, histocompatibility testing, or research studies related to immune system function and disease associations.
HLA-DQ alpha is a gene within the HLA complex, which is responsible for encoding proteins involved in the immune response. Variations in the HLA-DQ alpha gene can result in different alleles, and the presence of specific alleles may be associated with certain immune-related conditions or diseases.
DQ alpha testing is sometimes performed in cases of infertility to assess the compatibility between partners or to investigate potential immunological factors contributing to reproductive difficulties such as:
Immunological compatibility: The DQ Alpha gene is part of the HLA complex and plays a role in immune responses. Variations in DQ Alpha alleles can affect the immune system’s response to foreign substances. In cases where a woman’s immune system perceives her partner’s sperm or embryos as foreign, an immune response may be triggered, leading to difficulties in conception, implantation failure, or recurrent miscarriages. DQ Alpha genotyping can be used to assess the compatibility of DQ Alpha alleles between partners and identify potential immunological barriers to successful pregnancy.
HLA matching and embryo selection: In certain situations, DQ Alpha genotyping may be used alongside other HLA typing methods to evaluate HLA compatibility between partners. This information can be particularly relevant when considering embryo selection during assisted reproductive technologies, such as in vitro fertilization (IVF). Selecting embryos that are HLA-compatible with the parents can help reduce the risk of immune-related complications during pregnancy.
By analyzing the specific alleles of the DQ Alpha gene, DQ Alpha genotyping can provide insight into the immune compatibility between partners and help guide treatment decisions in cases of infertility. It can assist in identifying potential immunological barriers and determining appropriate interventions or treatments to optimize the chances of successful pregnancy.
The evidence regarding the association between HLA-DQ alpha compatibility and infertility is still relatively limited and research is continuing to establish if, and how significantly, it may influence fertility outcomes.
DQ Alpha genotyping is a specialised, non-routine diagnostic test typically performed by fertility specialists or reproductive immunology experts in specific clinical scenarios where immunological factors are suspected to contribute to infertility.
Browse our latest blog articles on reproductive immunology, immune-related infertility issues and keep up with our news at Life Clinic.

