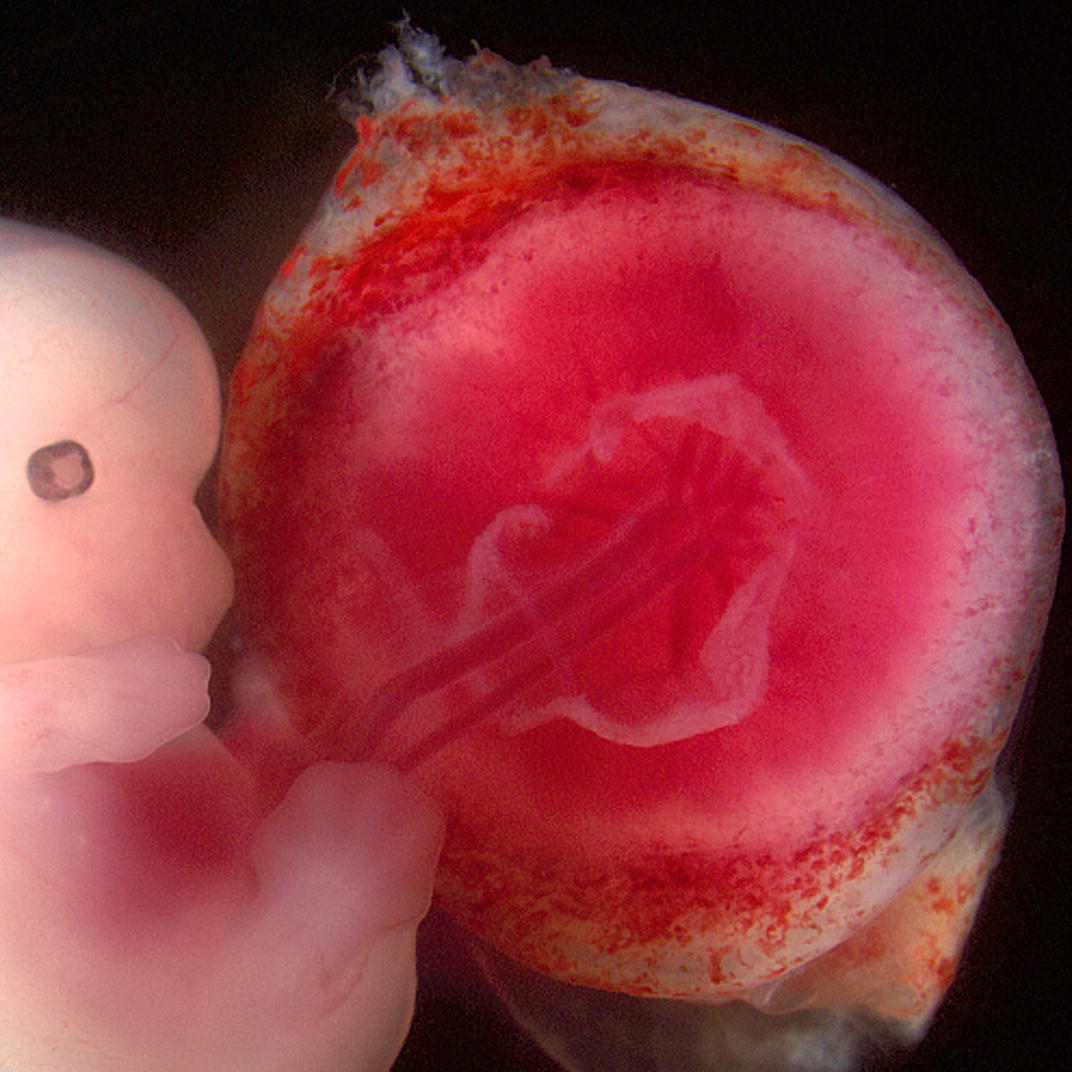
pregnancy
The immunological interaction between mother and fetus.
During pregnancy, the mother's immune system must strike a delicate balance between protecting the developing fetus from infection and avoiding rejection of the fetal tissue as a foreign invader.
Reaching this delicate balance requires a complex and highly regulated immunological interaction between the mother and fetus. One of the key mechanisms involved in this interaction is the establishment of immune tolerance. This is the process by which the mother’s immune system learns to tolerate the fetal tissue and not attack it as foreign. This is achieved through several mechanisms:
Placental barrier
The placenta acts as a physical barrier between the mother and fetus, preventing the mother’s immune cells from coming into direct contact with fetal cells.
Immunosuppressive factors
One of the key mechanisms of this immune tolerance is immunosuppression, which occurs at the site where the fetus attaches to the uterine wall, known as the placenta. The fetus and placenta produce various immunosuppressive factors that help to suppress the mother’s immune response.
- Fetal immunosuppression
During pregnancy, a reduced state of immune activity occurs in developing fetuses. The fetus produces a protein called HLA-G, which inhibits the function of maternal immune cells.
Additionally, the fetus itself has a developing immune system, but it is not fully mature or functional until after birth. This relative immaturity also contributes to fetal immunosuppression, as the fetus is not able to mount a strong immune response to potential pathogens or foreign substances.
- Placental immunosuppression
The placenta is an important site for immune regulation during pregnancy. One way that the placenta contributes to immunosuppression is by producing certain molecules that can suppress immune responses.
For example, the placenta produces high levels of a molecule called indoleamine 2,3-dioxygenase (IDO), which breaks down the amino acid tryptophan and limits the ability of immune cells to mount an inflammatory response. This helps to prevent the mother’s immune system from attacking the fetal tissue as a foreign invader.
In addition, the placenta also contains specialized immune cells called regulatory T cells (Tregs), which play a critical role in maintaining immune tolerance during pregnancy. Tregs suppress the activity of other immune cells that might otherwise attack the fetus, helping to prevent rejection.
Regulatory T cells
Regulatory T cells (Tregs) are a type of immune cell that helps to maintain balance in the immune system by suppressing or dampening the activity of other immune cells. They play a critical role in preventing excessive or harmful immune responses, such as autoimmune reactions or rejection of transplanted tissue.
Tregs are able to recognize and respond to “self” molecules in the body, which helps to distinguish between harmful invaders and healthy tissue. They also produce anti-inflammatory molecules that can help to reduce inflammation and tissue damage caused by other immune cells.
During pregnancy, the number and activity of Tregs increase, helping to suppress the mother’s immune response to the fetus. They are able to inhibit T cell proliferation and cytokine production and play a critical role in preventing autoimmunity.
Tregs play a key role in immune tolerance by acting to suppress immune response, thereby maintaining homeostasis and self-tolerance.
Natural Killer cells
Natural killer (NK) cells are a type of immune cell that can attack foreign or abnormal cells, including fetal cells. However, during pregnancy, the number and activity of NK cells are regulated to prevent them from attacking the fetus. (Read more about these cells below).
It is important to note that this immunological interaction between the mother and fetus is not foolproof, and problems can arise if the balance is disrupted. For example, if the mother’s immune system mounts an excessive response to the fetus, this can lead to pregnancy complications such as preeclampsia or miscarriage.
Conversely, if the immune tolerance mechanisms are too strong, this can allow infections or other problems to go unnoticed, potentially leading to fetal harm.
Elizabeth Pennisi, www.science.org, Nov 2018
Studies of single cells reveal complex interactions as placenta forms.
Understanding the complexity of the immune system could eventually help reduce miscarriages and other complications of pregnancy.
How the immune system attacks an embryo
In some cases, the immune system can mistakenly recognize the embryo as a foreign invader and mount an attack against it.
If an immune attack takes place it can lead to problems with implantation, fetal growth, and pregnancy complications. There are several mechanisms by which the immune system can attack an embryo:
Autoimmunity
Autoimmunity refers to a situation where the immune system mistakenly attacks the body’s own healthy tissues, organs, and cells as if they were foreign invaders. In other words, the immune system becomes confused and begins to recognize the body’s own tissues as foreign and harmful, leading to inflammation and damage.
An example of foetal autoimmunity is maternal lupus, which is an autoimmune disease in which the mother’s immune system attacks her own tissues. In some cases, the mother’s immune system may also attack the foetal tissues, leading to foetal distress, foetal growth restriction, or even foetal death.
Alloimmunity
Alloimmunity is a condition where the immune system of an individual reacts to and attacks foreign antigens present in another individual’s tissues or cells. In the case of alloimmunity in fetuses, it occurs when the mother’s immune system produces antibodies against the fetal tissues or cells, which are seen as foreign by the mother’s immune system.
This can happen when the fetus expresses certain antigens that are inherited from the father and are not present in the mother’s body. These antigens can be recognized as foreign by the mother’s immune system, leading to an immune response against the fetal cells expressing these antigens.
One common example of alloimmunity in fetuses is Rh incompatibility. This occurs when the mother is Rh-negative, and the fetus is Rh-positive, which means that the fetus has inherited the Rh antigen from the father, which the mother’s immune system does not recognize. If the fetus’s Rh-positive blood enters the mother’s bloodstream during pregnancy or childbirth, the mother’s immune system may produce antibodies against the fetal Rh-positive blood cells, leading to hemolytic disease of the newborn (HDN), which can cause severe anemia and jaundice in the newborn.
Another example of alloimmunity in fetuses is ABO incompatibility. This occurs when the mother has a different blood type than the fetus, such as when the mother is type O and the fetus is type A or B. The mother’s immune system can produce antibodies against the fetal blood cells expressing the A or B antigens, leading to HDN.
Autoimmunity and alloimmunity are both conditions that involve the immune system, but they are different in their underlying mechanisms and targets. In autoimmunity, the immune system targets self-antigens, while in alloimmunity, the immune system targets non-self-antigens.
Inflammation
Inflammation can cause damage to the fetus or placenta through various mechanisms. When the immune system recognizes a threat, it mounts an immune response, which often involves inflammation. Inflammation is a natural and necessary response of the immune system to fight off infection or injury. However, excessive inflammation can be harmful and may lead to damage to the developing embryo or placenta.
Inflammation can damage the fetus by disrupting the delicate balance of nutrients and oxygen that the fetus needs to grow and develop. Chronic inflammation can lead to a decrease in blood flow to the placenta, which can reduce the supply of oxygen and nutrients to the fetus. This can result in fetal growth restriction, which can cause long-term developmental and health problems.
Inflammation can also damage the placenta itself. The placenta is a complex organ that plays a crucial role in fetal development by providing oxygen and nutrients to the fetus and removing waste products. Inflammation can damage the placental tissue, leading to reduced placental function and impaired fetal development. Inflammation can also cause changes in the placental blood vessels, leading to decreased blood flow to the fetus.


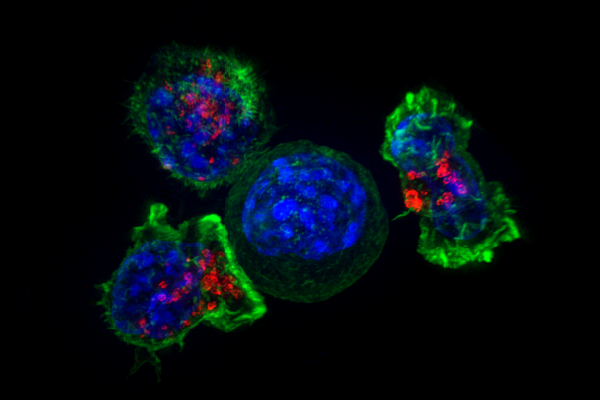
Natural killer (NK) cells
Natural killer (NK) cells are a type of immune cell that plays an important role in the defence against infections and cancer. In addition, NK cells also play a role in early pregnancy by regulating the implantation and development of the embryo. However, in certain cases, NK cells can also attack the developing embryo, leading to implantation failure and pregnancy loss.
During early pregnancy, to prevent rejection of the embryo, the mother’s immune system has to be modulated and tolerance to the embryo’s antigens established. NK cells are part of the mother’s immune system and are present in the uterus during early pregnancy. They play a critical role in establishing immune tolerance to the developing embryo.
In normal pregnancy, NK cells are activated by hormones and cytokines secreted by the embryo and placenta, leading to a shift towards a more tolerant phenotype. However, in some cases, the balance between maternal immune tolerance and activation is disrupted, leading to an excessive activation of NK cells. This can lead to the attack and destruction of the embryo, preventing successful implantation and development. The mechanism by which NK cells attack the embryo is not fully understood, but it is thought to involve the release of toxic substances that damage the embryo’s cells and tissues.
There are several factors that can contribute to the excessive activation of NK cells and their attack on the embryo, including genetic and environmental factors. For example, women with certain genetic variations in the genes that regulate NK cell function may be more susceptible to NK cell-mediated pregnancy loss. In addition, exposure to certain infections or inflammatory conditions can also trigger NK cell activation and attack on the embryo.

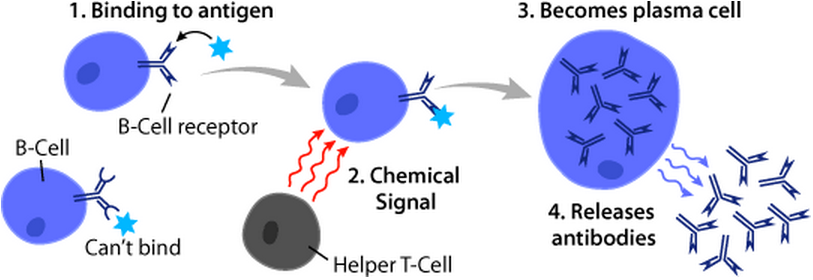
B cells
B cells are a type of white blood cell that plays a crucial role in the immune system. They are responsible for producing antibodies, which are proteins that can recognize and neutralize specific foreign substances, such as bacteria and viruses.
B cells are produced in the bone marrow and mature in the spleen and lymph nodes. When a foreign substance enters the body, B cells that are specific to that substance will recognize it and begin to produce antibodies. These antibodies then circulate throughout the body, binding to the foreign substance and marking it for destruction by other immune cells.
During pregnancy, the immune system suppresses the activity of certain immune cells, including B cells, to prevent them from producing antibodies that could potentially attack the fetus.
However, in some cases, B cells may become activated and produce antibodies against the fetus. This can occur if the fetus expresses certain antigens that are not present in the mother’s body or if there is a breakdown in the normal immune suppression mechanisms.
When B cells produce antibodies against the fetus, it can lead to a condition known as fetal alloimmune disease or hemolytic disease of the newborn (HDN). This can result in severe anemia, jaundice, and even death of the developing fetus or newborn.
Macrophages
Macrophages are an important component of the immune system and play a crucial role in protecting the body against infections. However, in certain cases, macrophages can also damage an embryo.
During pregnancy the immune system suppresses the release of macrophages to prevent them from attacking the developing fetus.
In newborn babies, this syndrome can significantly affect multiple organs with significant short and long term implications for the newborn.
Arch Dis Child Fetal Neonatal Ed. 2007 Mar; 92(2): F83–F88.
The changing management of haemolytic disease of the newborn is reviewed
Semin Fetal Neonatal Med. 2020 Aug;25(4):101146. doi: 10.1016/j.siny.2020.101146. Epub 2020 Oct 23.
The origins of a concept, pathophysiology, diagnosis, and obstetrical implications
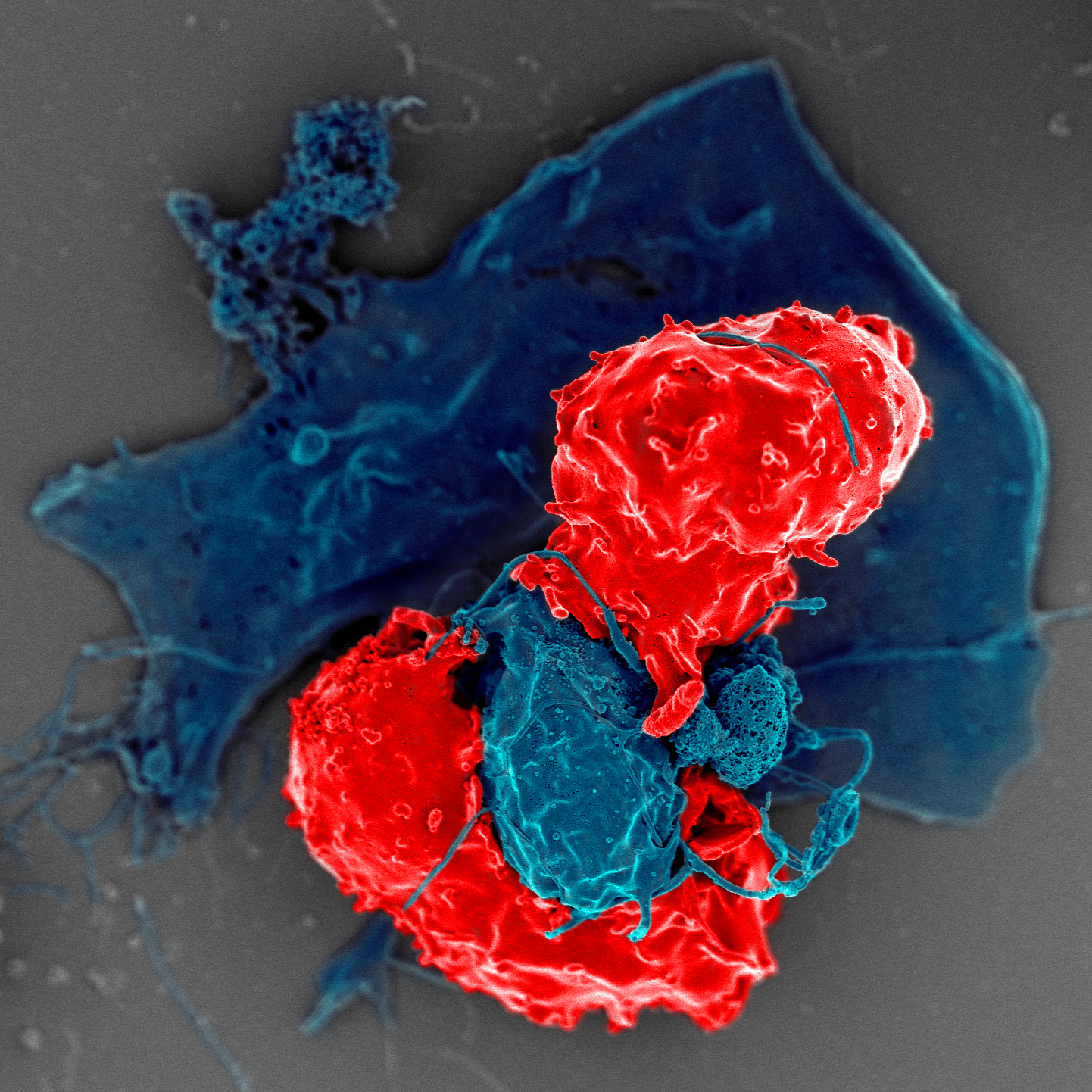
Professional killer cells
Natural killer (NK) cells play a role in defence against viral infections by killing infected cells or by producing cytokines and interacting with adaptive immune cells.
When a NK cell makes contact with a target cell, it attaches and spreads over the dangerous target. The NK cell then uses special chemicals housed in vesicles (red) to deliver the killing blow. This event has been named “the kiss of death”. After the target cell is killed, the NK cells move on to find the next victim.
NK cells are a type of white blood cell that play an important role in the immune system. They are part of the innate immune system, which is the body’s first line of defense against infections.
NK cells are called “natural killer” cells because they can identify and kill infected or abnormal cells without the need for prior exposure or activation. They do this by recognizing and binding to abnormal cells, such as virus-infected cells or tumor cells, and releasing toxic molecules that induce cell death.
In addition to their cytotoxic activity, NK cells also play a role in regulating the immune response by producing cytokines, which are signaling molecules that help coordinate the immune response. They can also interact with other immune cells, such as dendritic cells and T cells, to enhance their function and activation.
NK cells are derived from white blood cell precursors in the bone marrow and are present in tissues throughout the body, particularly in the blood, spleen, and liver.
They are important during pregnancy, as they can help regulate the development and function of the placenta and protect against infections. (Read more)

Which immune cells react against embryos
The immune system plays a critical role in protecting the body from infection and disease. However, dysregulation or abnormalities in the immune system can lead to pregnancy complications.
There are several types of immune cells that can be involved in the immunological reaction against an embryo, including:
- Natural killer (NK) cells: NK cells are a type of immune cell that can attack foreign or abnormal cells, including fetal cells. (Read more)
- T cells: T cells are a type of immune cell that play a key role in the immune response. Some studies suggest that abnormalities in T cell populations and functionality may be involved in pregnancy complications such as recurrent miscarriage.
- B cells: B cells are another type of immune cell that produce antibodies, which can target foreign or abnormal cells. In some cases, antibodies produced by B cells may mistakenly target fetal cells, leading to pregnancy complications. (Read more)
- Macrophages: Macrophages are immune cells that play a role in inflammation and tissue repair. In some cases, abnormal macrophage activity may contribute to pregnancy complications. (Read more).
The exact mechanisms by which these cells contribute to the immunological reaction against an embryo are not fully understood. However, it is thought that they may recognize certain proteins or antigens on the surface of the embryo or placenta as foreign, leading to an immune response that can damage or destroy fetal cells.
In some cases, the immune system may also attack the cells of the maternal-fetal interface, leading to problems with implantation and placental development.
immunological reactions
Coagulation abnormalities
The immune system and coagulation system are closely linked, and abnormalities in one system can affect the other.
During pregnancy, there is a delicate balance between coagulation and anticoagulation factors to prevent excessive bleeding while still allowing blood flow to the developing fetus. However, in some cases, this balance can be disrupted, leading to hypercoagulability (increased clotting) and an increased risk of complications such as miscarriage, pre-eclampsia, and fetal growth restriction.
The immune system can also play a role in coagulation by producing pro-inflammatory cytokines, such as TNF-alpha and interleukin-6, that can increase clotting factors and decrease the activity of anticoagulant proteins such as protein C and protein S. This can lead to a prothrombotic state and an increased risk of thrombosis (blood clots).
Furthermore, some autoimmune disorders, such as antiphospholipid syndrome, can lead to the production of antibodies that target proteins involved in coagulation, leading to a higher risk of blood clots and pregnancy complications.
Fertility and Sterility Vol. 106 Issue 3 p497–498 (2016)
The immune system plays an irrefutable role in normal fertility and successful applications of immunology have become standard part of evidence-based clinical practice. The field of reproductive immunology will clearly be a future source of significant improvement in the prevention and treatment of many reproductive disorders…
Science Immunology; Vol 2, Issue 15 (2017)
On the Clock. During pregnancy, the mother’s organ systems, including her immune system, adapt to the growing fetus.
Aghaeepouret al. chart immune system adaptations during the course of a human pregnancy. This immunological time line is critical for healthy mothers and babies.
TedTalk, Lauren St-Germain, PhD researcher, UBC (2021)
In this talk, Lauren St-Germain discusses reproductive immunology and how immune imbalance can make pregnancy less healthy and cause complications.
In pregnancy, the mother’s womb is commonly thought to be a safe and nurturing environment; but in reality, it’s a warzone.
Our story
Signs of an abnormal immune system
Abnormal immunological reactions during pregnancy can lead to a variety of complications that may affect both the mother and the developing fetus.
Such immune reactions may not always cause symptoms that are noticeable to the mother. In other cases, an immune reaction can lead to symptoms including Recurrent miscarriage, Abnormal vaginal bleeding, Abnormal placenta development, Preterm labor, Intrauterine growth restriction and others.