
 IN THE NEWS –
IN THE NEWS –
Research indicates that the endometrium is immune sensitive and responsive.
The endometrium is an immunologically modulated tissue for microbiota and possible regulator of inflammatory and immune responses. A recent study highlights the current scientific understanding of the endometrium and its pivotal tole in reproduction with specific regard to immune responses and microbiota.
Research Paper: (READ FULL ARTICLE)
Molina, N. M., Sola-Leyva, A., Saez-Lara, M. J., Plaza-Diaz, J., Tubić-Pavlović, A., Romero, B., … & Altmäe, S., (2020), ‘New Opportunities for Endometrial Health by Modifying Uterine Microbial Composition: Present or Future?’, Biomolecules, 10(4), 593. [doi:10.3390/biom10040593]

Some background first…
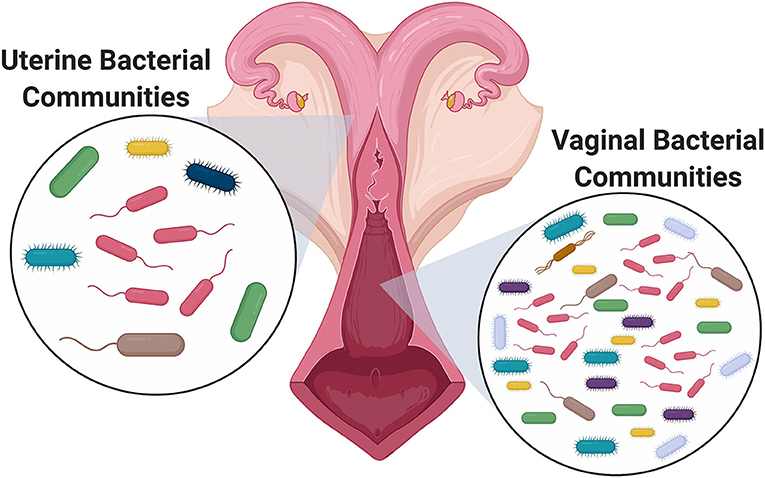
Until recently the uterine cavity was believed to be a sterile environment due to the present of the cervical plug (it has actually been compared to the “Colossus of Rhodes” in the sense that it was thought to provide an impermeable barrier to bacteria in the vagina). However, this is no longer known to be the case, since it was discovered that the cervical plug was not entirely impermeable. With the advent of new technologies (next-generation sequencing (NGS)), scientists have been able to detect and identify bacteria in the uterine cavity. The endometrial (or uterine) microbiome in humans has a low bacterial diversity. The low diversity is due to a single genus, named Lactobacillus, accounting for the majority of the bacteria. Many factors, such as ethnicity, age and inflammation, can influence the composition of this microbiome.
The presence of bacteria helps to keep the uterine cavity healthy by taking in molecules and breaking them down through metabolic processes. Additionally, other components are released into the uterus that contributes to the health of the microbiome by supporting the functions of other bacteria, adjusting the pH of the environment, and regulating the functions of immune cells. The regulation of immune cells helps to fight off pathogens as well as create an environment in the uterus that helps support pregnancy development.
Source: ‘Bacteria in the Reproductive Tract: They Are Not All Bad!’ (Frontiers, February 25, 2021)
Studies have shown that shifts in the composition of this endometrial microbiota can impact fertility (through inflammatory responses, implantation failure and immune response), women’s health (causing certain gynaecological disorders) as well as maternal & fetal health during pregnancy.
![]() A healthy endometrium is the foundation for successful implantation.
A healthy endometrium is the foundation for successful implantation.
A woman’s uterus is lined with endometrial tissue. This lining is called the endometrium. The physiological functions of the endometrium are preparation for implantation, maintenance of pregnancy if implantation occurs, and menstruation in the absence of pregnancy.
![]() RESEARCH HIGHLIGHTS –
RESEARCH HIGHLIGHTS –
Possible function of microbes in the uterus and the immunological functions of the endometrium in modulating inflammatory and immune responses.
Inflammatory responses to bacterial changes are thought to be related to infertility. For example, several studies have shown an increased number of immunoglobulins (IgM, IgA, and IgG) in patients with chronic endometritis (CE) and Recurrent Implantation Failure (RIF) [1]. Also, studies in patients with endometriosis have detected significantly higher levels of the proinflammatory cytokines interleukin 6 (IL-6), proIL-1β, and IL-1β occurring.
 The understanding of what constitutes healthy endometrial microbiota and how changes in its composition affect immune responses and fertility could allow personalised treatment through microbiome management during assisted reproduction treatments.
The understanding of what constitutes healthy endometrial microbiota and how changes in its composition affect immune responses and fertility could allow personalised treatment through microbiome management during assisted reproduction treatments.

Keywords: endometrial microbiota, uterus, infertility, assisted reproductive technologies, immune response, inflammation, Recurrent Implantation Failure
 References:
References:
[1] Toson, B., Simon C., Morenom, I., ‘The Endometrial Microbiome and Its Impact on Human Conception’, Int J Mol Sci. 2022 Jan; 23(1): 485, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8745284/]
[2] Molina, N.M. et al., ‘Review: New Opportunities for Endometrial Health by Modifying Uterine Microbial Composition: Present or Future?’, 11 April 2020, Journal: Biomolecules 2020
